Smart Prosthetic Prototype
The Problem:
In order to be fit for a prosthetic, a patient endures a fitting process spanning a couple months. The prosthetist relies on a relatively crude technique to fit a prosthetic socket to a patient: scrawling lipstick on the patient's stump in order to identify contact points in the socket mould. Amputees also suffer from residual limb volume loss, requiring intermittent resizing appointments.
The Solution:
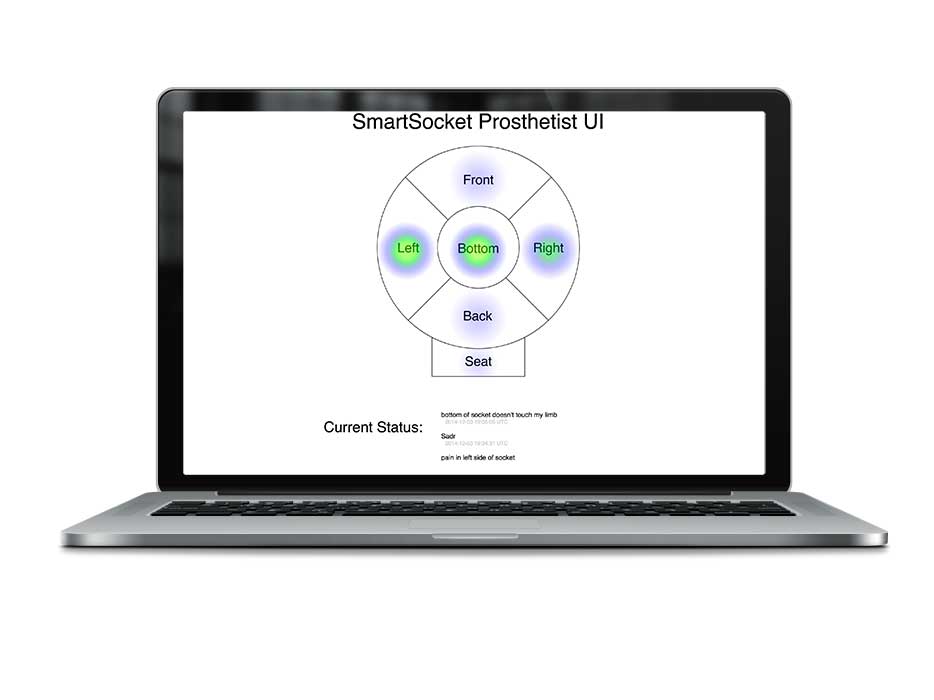
Working with a prosthetic start-up company in the Bay Area, we incorporated force sensors into the socket cup and ischial seat of their prosthetic prototype. The data gathered through the sensors were then sent to an Android device via BLE technology. The resulting output can be viewed by the patient's prosthetist, allowing for a more informed fitting. The prosthetist, in turn, is also able to monitor the magnitude of residual limb volume changes and to perform preventive care by identifying points of contact that may cause too much pressure.
The Process:
As part of the final project for an Interactive Device Design course at UC Berkeley, I co-led a multidisciplinary team (Josh Stroud, Peter Gao, and myself) and followed a human-centered design thinking process to integrate user feedback and observations in order to generate informed design principles, brainstorming sessions, and concept ideation.
Through an interview with a prosthetist, one who fits patients with a prosthetic socket, we learned that the common method of fitting a patient with a prosthetic socket is relatively crude; lipstick is scrawled on a patient’s stump in order to see points of contact within the socket cup. These contact points inform the prosthetist of how to create an improved fit.
We interviewed amputees and prosthetists. Both of the amputees interviewed were active and competed in running events. Thus, the team used these interviewees as models for our persona generation: a young tech-savvy professional who likes to be able to be on the move, able to wear their prosthetic throughout a work day, and be able to compete in distance running events. They also commented how ease of cleaning and removal was essential. This meant that we needed to ensure the addition of sensors and electronics enclosure integration could be easily removed and would not negatively impact user mobility.
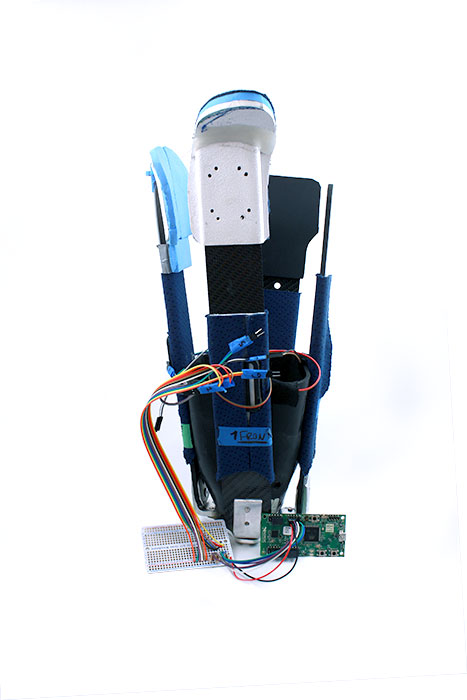
We developed a smart prosthetic to enable prosthetists to create a better fit for patients. This results in an improved experience not only during the fitting process but also an overall improved experience for a patient while using their prosthetic. The device used 6 sensors; 4 on each strut of the prosthetic; 1 that rests in the bottom of the cup; and 1 that rests at the ischial seat.
The data measured from the force-sensitive resistors (FSR) are transmitted through Bluetooth Low-Energy (BLE) to the cloud. This data is then accessible by either a web or mobile UI. This data visualization allows prosthetists to 'see' what areas within the cup need more (or less) support. If given more time, we would like to conduct user tests and create additional iterations. We would also like to make the electronics enclosure smaller as well as explore additional use-cases of the device.